Uninsured rates are down following coverage expansions, but gains have stalled, and in some states have begun to erode
16
States uninsured rates for working-age adults ticked up one percentage point between 2016 and 2017
The 2019 State Scorecard found that the historic gains made by states in expanding health insurance coverage and access to care following the Affordable Care Act’s major coverage expansions in 2014 have stalled or even begun to erode in some states.
States’ historic progress in expanding health insurance coverage and access to care has stalled
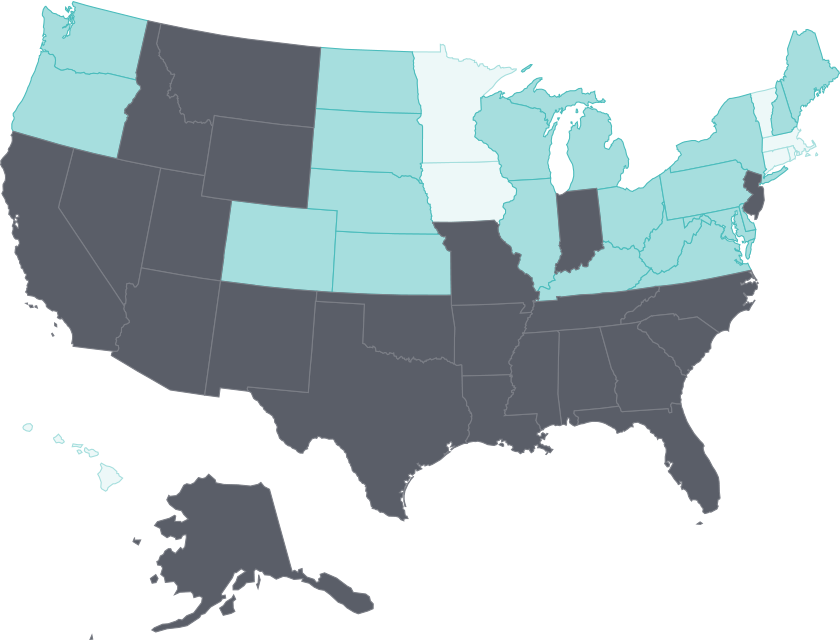
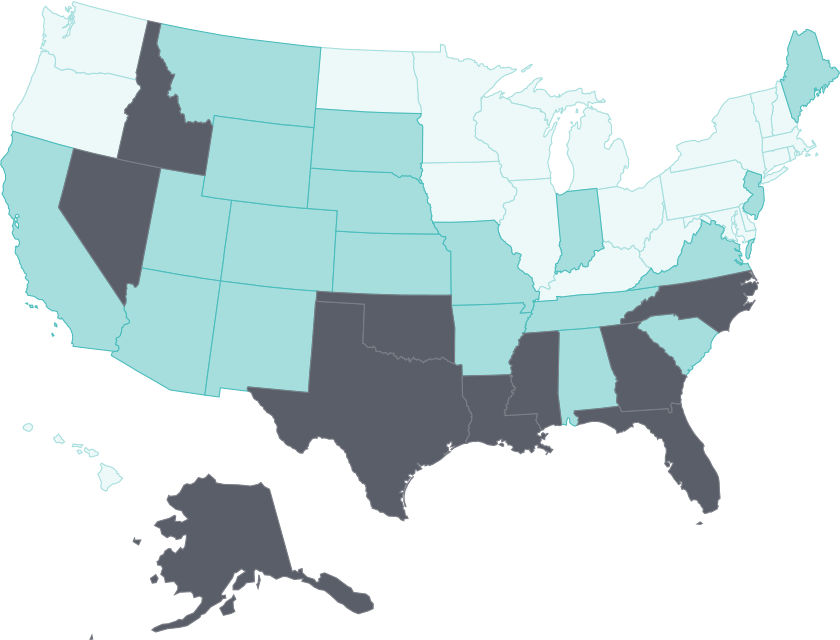
In nearly all states, there were widespread reductions in uninsured rates between 2013 and 2017, in the wake of the ACA’s insurance market reforms and coverage expansions (Exhibit 5, Appendix C2).
As more people gained coverage, fewer cited cost as a barrier to receiving needed care. But in most states, progress stalled after 2015. From 2016 to 2017, more than half of states simply held on to earlier gains; 16 states, including those that did and did not expand Medicaid, experienced upticks of 1 percentage point in their adult uninsured rate (Appendix C3).7 One notable exception was Louisiana, where Medicaid expansion took effect in July 2016. Louisiana experienced a 3 percentage-point drop in its adult uninsured rate (from 15% to 12%) from the end of 2016 to the end of 2017. People with low income made the greatest gains (Appendices C3 and C4).
Cost barriers to receiving care fell as uninsured rates fell following ACA coverage expansions
- Select a year to see changes over time.
Uninsured adults
2013 Adults who went without care because of costs
2013
- Less than 10%
- 10%-14%
- 15% or more
Notes: Adults who went without care is limited to adults ages 18–64 in this exhibit, though the Scorecard ranks states on a version of this measure that includes all adults age 18 and older.
Data: Uninsured (ages 19–64): U.S. Census Bureau, 2013–2017 One-Year American Community Surveys, Public Use Micro Sample (ACS PUMS); Cost barriers (ages 18–64): 2013–2017 Behavioral Risk Factor Surveillance System (BRFSS).
Share
Medicaid makes a difference in lowering uninsured rates
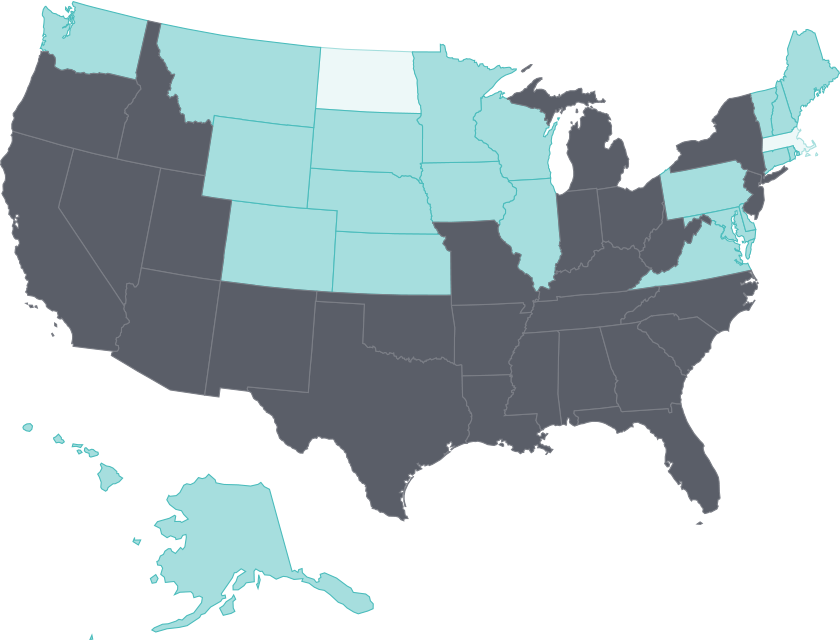
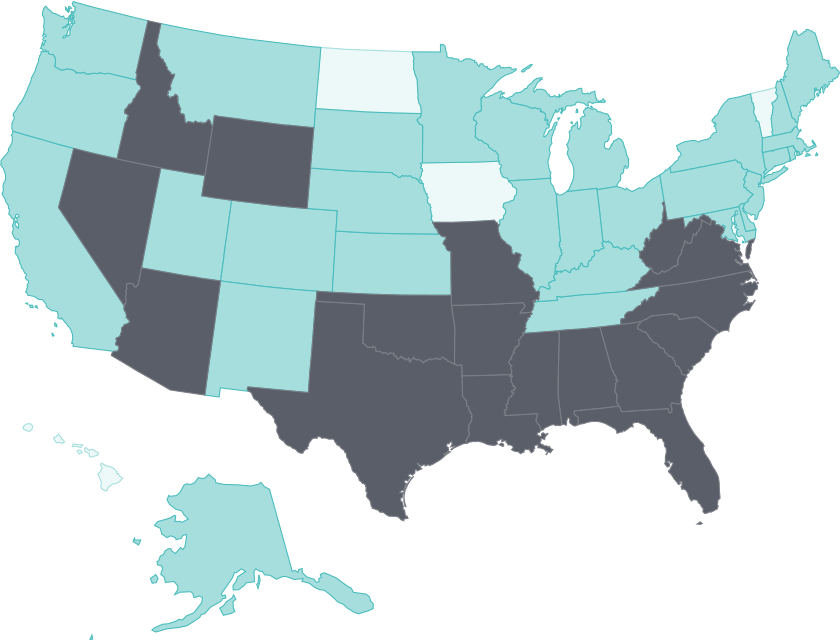
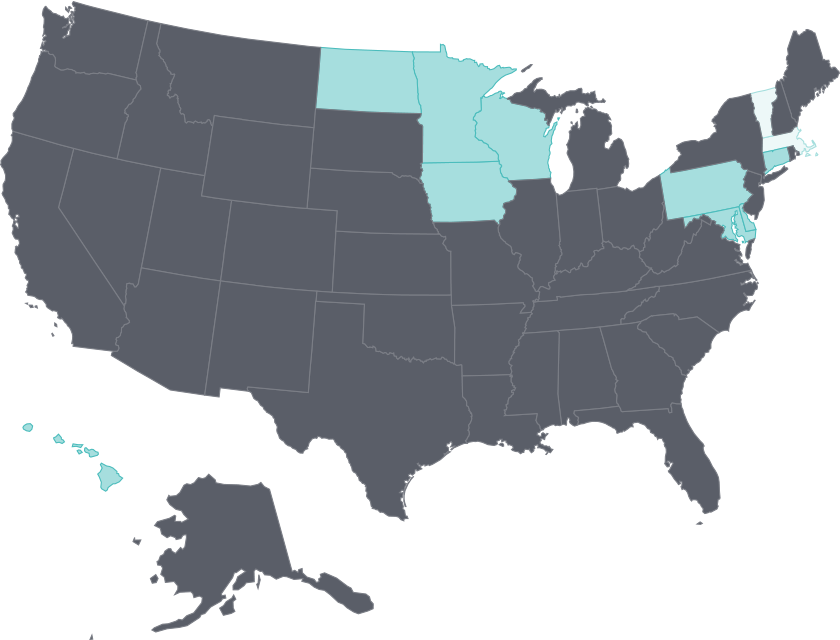
States’ decisions about whether to expand their Medicaid programs have had stark implications for their uninsured rates.
This is apparent in the sixfold variation across state uninsured rates in 2017, ranging from a low of 4 percent in Massachusetts (which expanded Medicaid along with coverage enhancements like extra subsidies) to a high of 24 percent in Texas (which did not expand) (Exhibit 6, Appendix C2). Among the 17 states that have yet to expand Medicaid, five had the highest uninsured rates, ranging from 18 percent to 24 percent.
Five of the 17 states that have yet to expand Medicaid had the highest adult uninsured rates in 2017
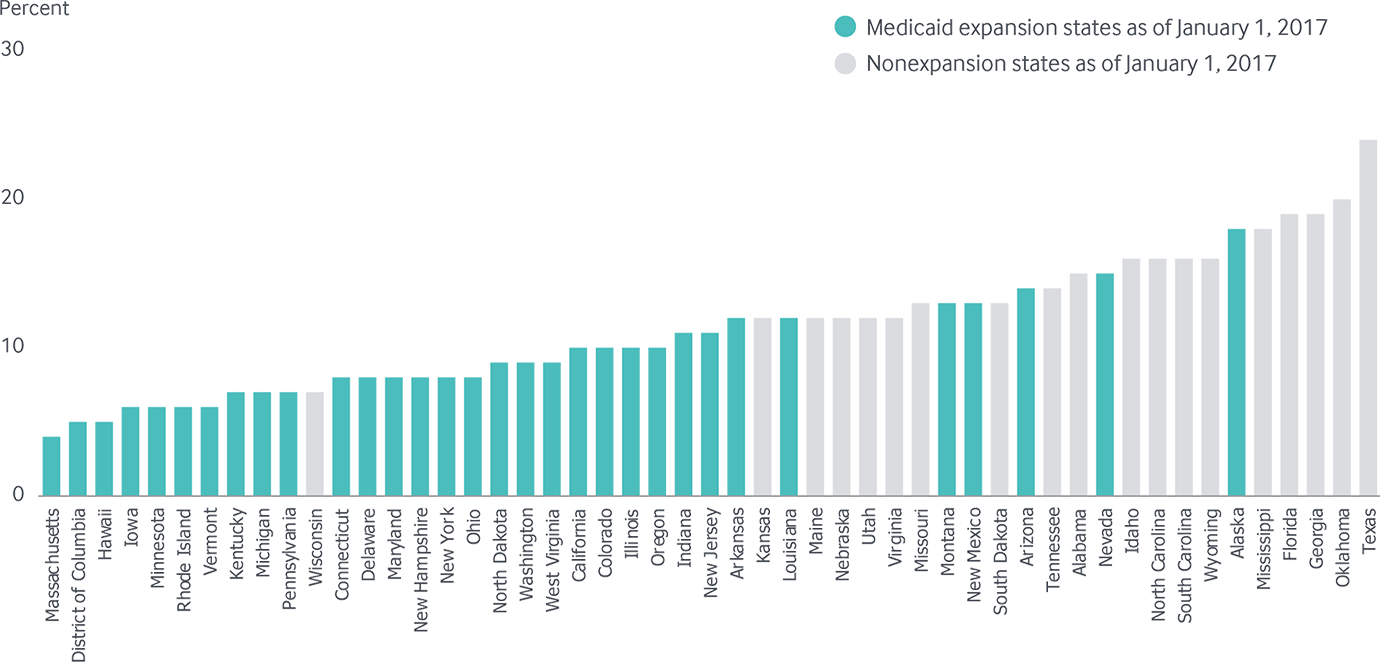
Note: As of January 1, 2017, there were 19 states that had not expanded Medicaid. Maine and Virginia implemented Medicaid expansion in 2019; Idaho, Nebraska, and Utah passed ballot initiatives in November 2018 to expand Medicaid but have not yet implemented a full expansion; Utah made adults up to 100% of poverty eligible. Adults with incomes up to 100% of poverty are eligible for Medicaid in Wisconsin.
Data: U.S. Census Bureau, 2017 One-Year American Community Surveys. Public Use Micro Sample (ACS PUMS).
Share
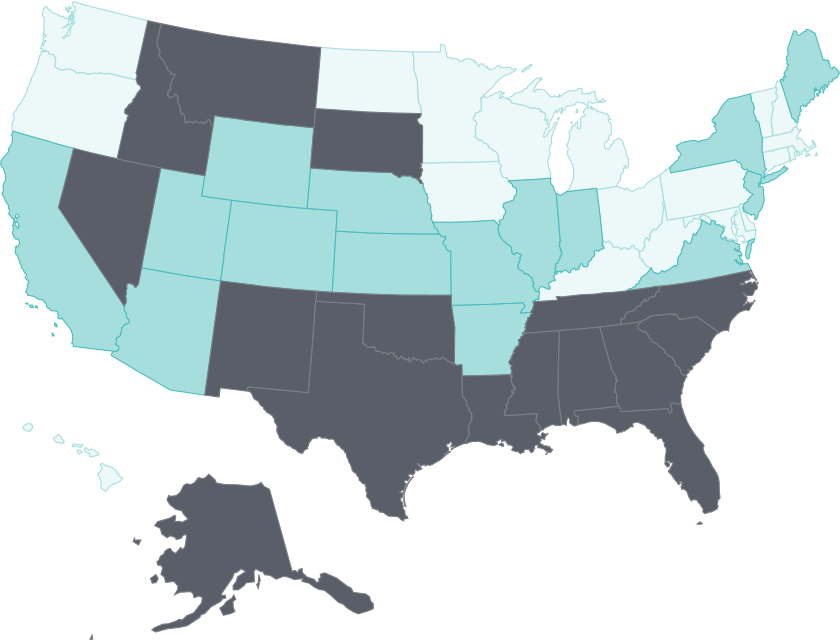
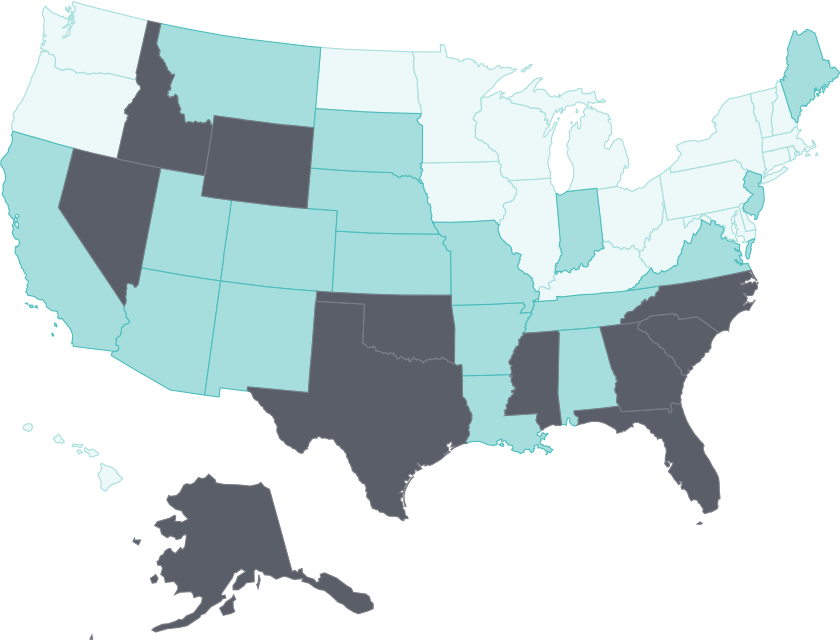
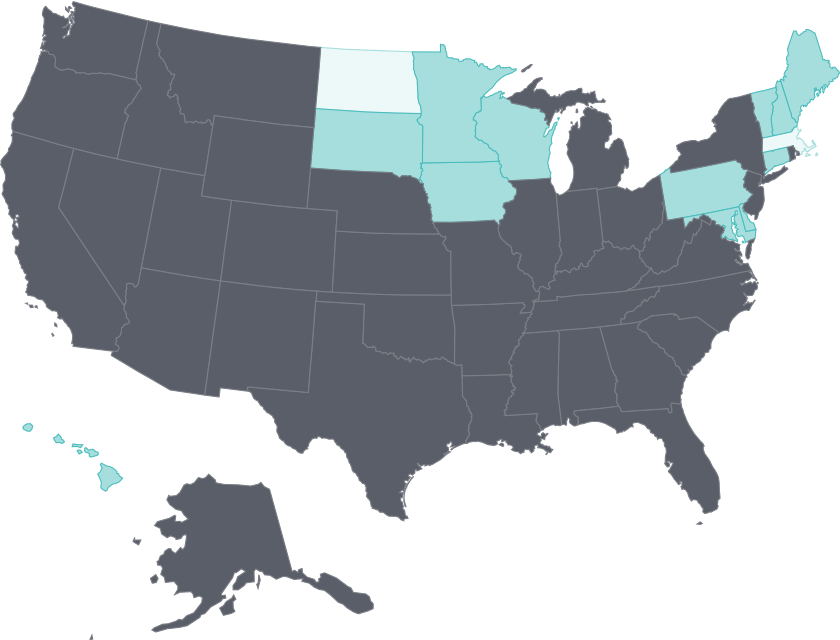
In states that recently expanded Medicaid, uninsured rates among low-income adults dropped substantially in 2017
All states saw reductions in uninsured rates among low-income adults following the ACA’s 2014 coverage expansions, with states that expanded Medicaid seeing the largest drops. After falling through 2015, state uninsured rates among low-income adults did not change much between 2016 and 2017 (Exhibit 7).
The notable exceptions to this trend were three states that expanded Medicaid in 2015 or later: Alaska (September 2015), Louisiana (July 2016), and Montana (January 2016). Uninsured rates among low-income adults in these states dropped by 8, 6, and 4 percentage points, respectively, from the end of 2016 to the end of 2017. These gains suggest the potential for improving uninsured rates among low-income adults in the latest batch of states that have either expanded Medicaid (Maine and Virginia in 2019) or are poised to (Idaho, Nebraska, and Utah passed ballot initiatives in November 2018 to expand the program). In contrast, the failure of a November ballot initiative in Montana to permanently reauthorize the state’s full Medicaid expansion, which was due to “sunset” this summer, and subsequent legislation that would impose work requirements for enrollees, could endanger recent gains made there.8 In Wyoming, Montana’s neighbor — which has not expanded its Medicaid program — a third of low-income adults were uninsured in 2017.
Uninsured rates among people of color are also high in several of the states that have yet to expand Medicaid and are home to large African American and Hispanic populations. In Florida, Georgia, and Texas, for example, about 20 percent of black adults were uninsured in 2017, above the U.S. average of 14 percent (Appendix C3). More than a third of Hispanic adults in Texas and close to half of Hispanic adults in Georgia were uninsured in 2017. By contrast, uninsured rates among Hispanic adults in New York and in California, two states that did expand Medicaid, were 16 percent and 17 percent, respectively.9
States that more recently implemented Medicaid expansion saw the biggest drops in uninsured low-income adults in 2017
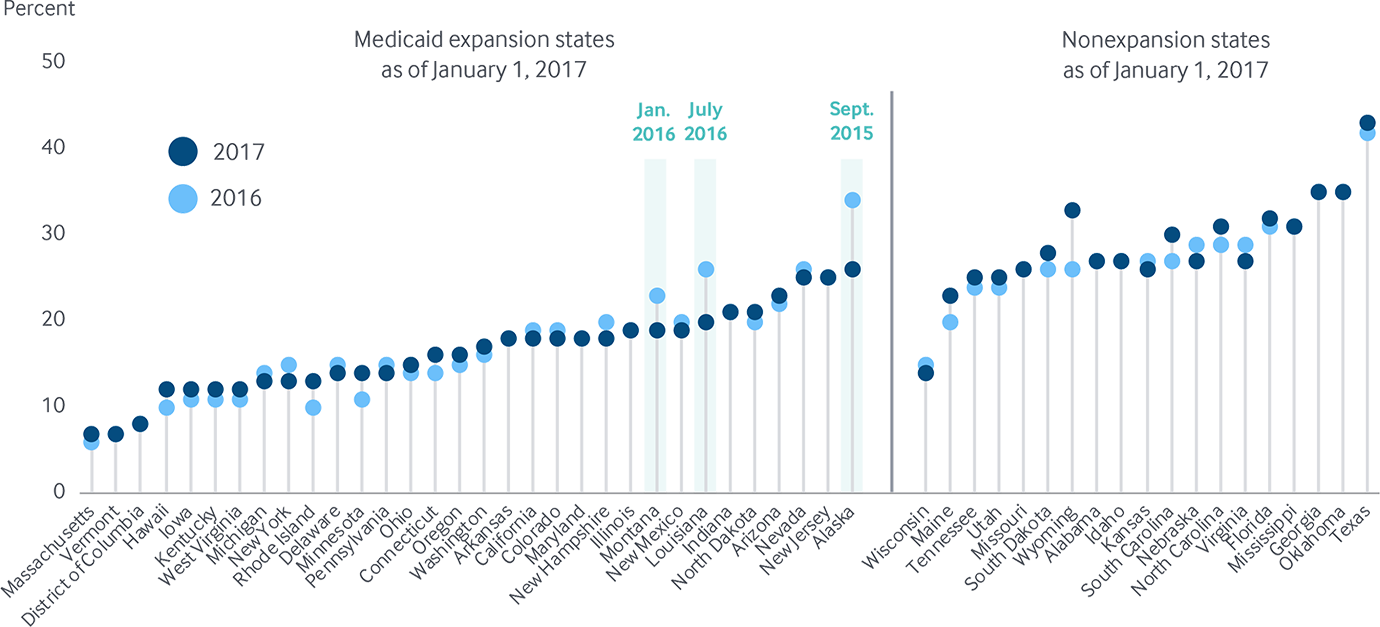
Notes: Low-income adults defined as adults ages 19–64 living in a household with income <200% of the federal poverty level. Medicaid expansion states are those states that expanded Medicaid by January 1, 2017. States arranged in order of their 2017 rate.
Data: U.S. Census Bureau, 2017 1-Year American Community Survey, American FactFinder and 2016 1-Year American Community Surveys, Public Use Micro Sample (ACS PUMS).
Share
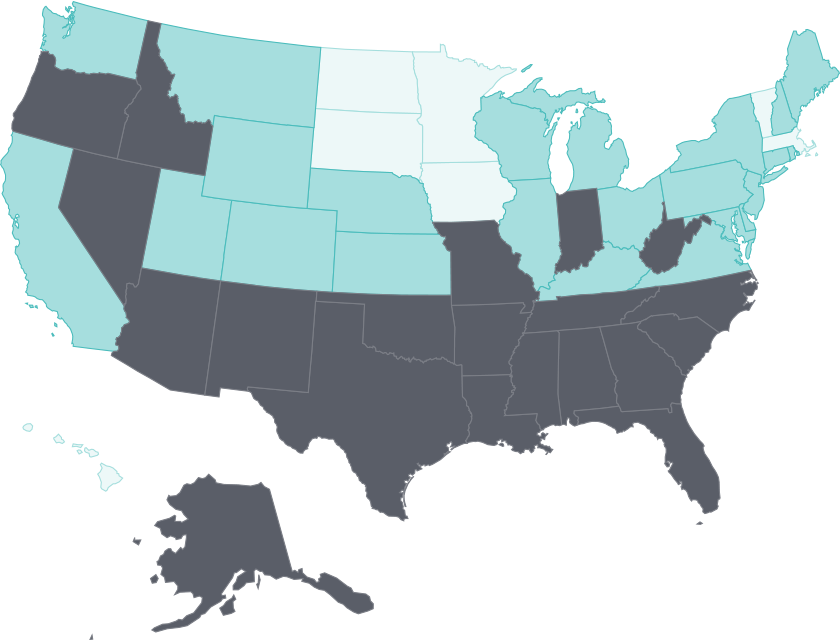
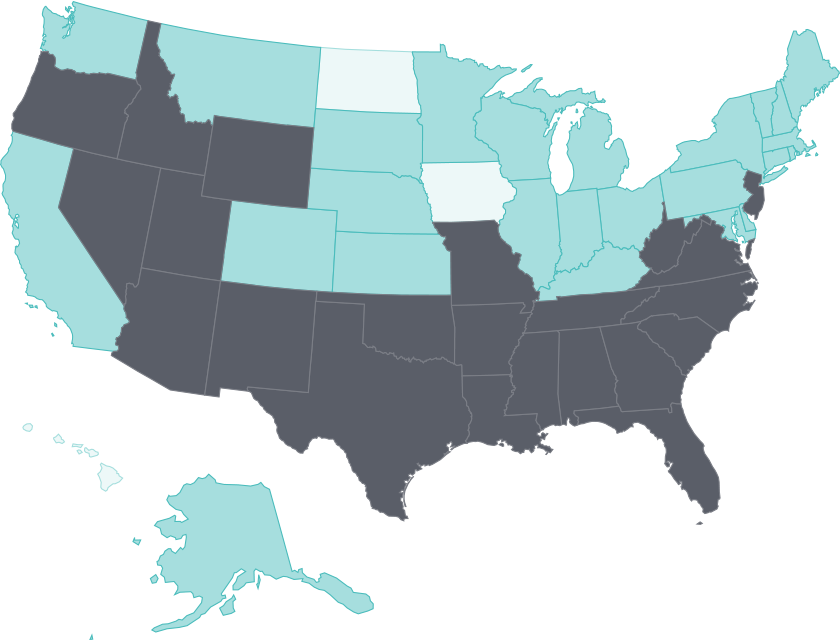
Cost barriers to care on the rise
As the progress in expanding health coverage stalled, so too did gains in people’s ability to access health care. Between 2016 and 2017, a dozen states had increases of at least 2 percentage points in the share of adults ages 18 to 64 who reported they had not gone to the doctor when needed because of cost (Exhibit 8).10
But it’s also worth noting that as with uninsured rates among low-income adults, some states that expanded Medicaid after 2014 saw a decrease in the share of adults in this income group who skipped needed care because of cost between 2016 and 2017. In Alaska, for example, the rate of low-income adults who went without care because of cost dropped from 31 percent in 2016 to 13 percent in 2017; in Louisiana, the rate dropped from 37 percent to 28 percent (Appendix C4).
The share of adults ages 18–64 who skipped needed care because of cost climbed by 2 percentage points or more in a dozen states between 2016 and 2017, eroding earlier gains
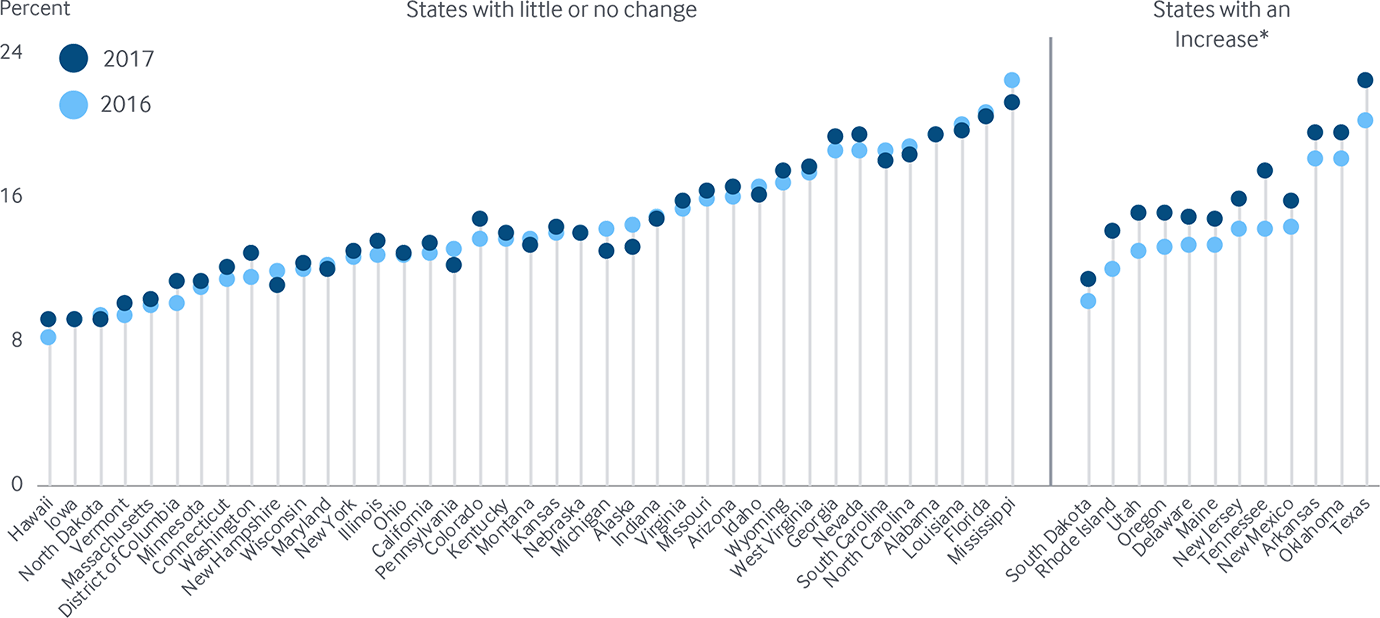
Note: States are arranged in rank order based on their 2016 value. * Rate increase refers to change between 2016 and 2017 of at least 2 percentage points. Adults who went without care is limited to adults ages 18–64 in this exhibit, though the Scorecard ranks states on a version of this measure that includes all adults age 18 and older.
Data: 2016 and 2017 Behavioral Risk Factor Surveillance System (BRFSS).